PRESENTATION ON
CMC, POST APPROVAL REGULATORY AFFAIRS.
REGULATION FOR COMBINATION PRODUCT AND
MEDICAL DEVICES.
PRESENTED BY:
RUBI PARVEEN
M. PHARM(PHARMACEUTICS)1ST YEAR
SCHOOL OF PHARMACEUTICAL EDUCATION AND RESEARCH(SPER)
JAMIA HAMDARD
CONTENT
➢ INTRODUCTION
➢ CMC
➢ POST APPROVAL CHANGES
➢ REGULATION FOR COMBINATION PRODUCT
AND MEDICAL DEVICES.
❖CMC REGULATORY AFFAIRS
CMC stands for Chemistry ,Manufacturing and Control.
To conduct clinical investigation and market
pharmaceutical product, companies are legally required
to obtain and maintain regulatory approval.
Regulatory affair is a discipline and strategic function
within the overall organization structure of
pharmaceutical company that directly interact with
government regulatory agency concerning RA.( FDA,
PMDA).
They ensure the compliance of cGMP, GLP and clinical
practice.
➢ CMC is relatively small section (approx 15-20%) of a (NDA),
but it often becomes a reason to delay in the approval of
NDA/Biologics licensing application(BLAs).
➢For ANDA, CMC section is significant(around 80- 90%), it is
important section in post approval life cycle management of the
products.
CMC REGUALTORY AFFAIRS
➢ Government regulatory agencies involved in the approval process
are:-
1. The food and drug administration(FDA)
2. European medicines agencies (EMA)
3. Japanese Pharmaceuticals and Medical Device Agencies(PMDA)
➢ CMC(RA) is a specific area with in RA, that has the ultimate
responsibility for providing, strategy required to achieve regulatory
approvals.
➢ As a strategic function, CMC RA collaborates closely with multiple
scientific, technical, quality, and commercial areas within a
company or with external contract manufacturing
organization(CMOs).
➢ Information regarding CMC for drug is important and detailed
section in a dossier to support clinical studies and marketing
application and this information should be updated throughout
drugs lifecycle.
REGULATION
21 CFR 312.23(a)(7)(i)
Appropriate for the particular investigation covered by IND ,A
section describing the composition, manufacture and control of the
drug substance and the drug product sufficient CMC information
to assure the proper identification, quality, purity and strength of
investigational drug.
1. CMC REVIEW AT IND STAGES
✓Primary objective is to assure the safety of patients, during all
phases of the IND.
✓PHASE 1 CMC evaluated mainly from the point of risk to
patient.
✓PHASE 2 and 3 CMC evaluates safety and additionally the
linkage of the clinical test product to be marketed product.
❑ POST PHASE 1 SUBMISSION
Continue to provide CMC data to support clinical studies.
Develop data for future NDA submission
Demonstrate that to- be-marketed drug has the same
identity, purity and strength as that the investigational drug
proven to be effective and safe through clinical studies.
Demonstrate consistency and reliability of drug
manufacturing process over product life.
❑CMC REGULATORY SUBMISSION
❑ CMC regulatory submission are not limited to
information associated with the API and finished dosage
form, it contains:-
Name and location of the manufacturing and testing
sites.
Characterization of API and composition of the dosage
form.
Description of the product and process development.
Description of the manufacturing process.
Analytical method used for testing and release of raw
material.
in progress controls, container and closure system.
stability testing Data for both the API and dosage form.
❑CMC REGULATORY SERVICES
Preparation and review of regulatory submission including
:-
Investigation new drug (IND)
Clinical trial authorization(CTA)
Investigational medical product dossier(IMPD)
New drug application (NDA)
Marketing authorization application(MAA)
Abbreviated new drug application(ANDA)
Authority of annual reports, drug master files, dossier
amendments and supplements
Preparation , publication and submission of eCTD
application( electronic common technical documents).
Direct interaction and negotiation with U.S. FDA, EMA
and national agencies.
❑ CMC SPECIALITIES IN PHARMACEUTICAL AND
BIOPHARMACEUTICAL INDUSTRIES
Interpretation and application of CMC regulatory regulations and
guidance for IND, NDA and DMF.
CMC regulatory strategy development and implementation
including of quality, safety and efficacy.
CMC regulatory planning, preparation, and participation for FDA or
EMA meetings.
CMC regulatory problem solving related to API, drug product,
dosage form, contract manufacturing organization (CMO).
POST APPROVAL REGULATORY
AFFAIRS
The FDA may require a post approval study at the time
of approval of pre market approval(PMA) , humanitarian
device exemption(HDE) or product development
protocol(PDP) application to help assure continued
safety and effectiveness of the approved drug product of
medical device.
For sponsors failure to comply with any post approval
requirement may be grounds for withdrawing approval
i.e. whether the post approval study will be terminated or
revised/replaced.
✓ Holders of NDA and ANDA who intended make post approval
changes should follow section506 A of the federal food , Drug and
Cosmetic act.
✓ Which provides requirements for making and reporting
manufacturing changes to an approval application and for
distribution changes.
✓ An application must provide specific information to access the
effect of the quality, purity and potency of a drug product.
❑ REPORTING CATAGORIES –
1. MAJOR CHANGE – substantial potential
2. MODERATE CHANGE – moderate potential
3. MINOR CHANGE- minimal potential
1. MAJOR CHANGE-
• Major change may require the submission of a supplement and
approved by FDA prior to distribution of the product.
• This type of supplement is called, prior approval supplement.
And applicant may ask FDA to expedite its review of prior
approval supplement for public health reason.
• This type of supplement is called , prior approval supplement
– expedite review requested.
2. MODERATE CHANGE- Two type of moderate change are
there-
• One type of moderate change may requires the submission of
supplement to FDA at least 30 days before the distribution of the
drug product.
• This type of supplements called , and should be clearly labeled a
supplement changes being effected in 30 days.
• FDA inform applicant within 30 days if the information is
missing distribution must be delayed, until supplement
amended, this type of supplement called and clearly labeled,
a supplement – changes being affected.
• If after review, FDA disapprove it may order the
manufacturer to cease distribution of the drug product made
using disapproval changes.
3. MINOR CHANGES –
In annual report the list should be included in the summary
section.
❑ EQUIVALENT-
Comparing test results from pre and post changes material
and determining if the results are equivalent.
❑ ADVERSE EFFECT-
Some manufacturing changes have an adverse effect on
identity, strength, quality, purity f the drug product
❖ RECOMMENDATION ARE PROVIDED FOR POST
APPROVAL CHANGES –
1. Component and composition.
2. Manufacturing sites.
3. Manufacturing process.
4. Specification.
5. Container closure system.
6. Labeling.
7. Miscellaneous changes and
8. Multiple related change
1. COMPONENT AND COMPOSITION-
Qualitative and quantitative changes considered major changes
requiring a prior approval supplement.
2. MANUFACTURING SITE-
✓ Major changes- move different manufacturing site except one-
▪ Never inspected by FDA.
▪ doesn’t have cGMP compliance.
✓ Moderate change for manufacturing site –
A move to a different manufacturing site for the primary
packaging of any drug product.
✓ Minor change for manufacturing site-
Move a different manufacturing site for the secondary
packaging, and move a different manufacturing site for
labeling.
3. MANUFACTURING PROCESS-
a. Major change –
▪ changes that may affect drug product sterility, assurance
including- changes in the sterilization method.
e.g. gas , dry heat, irradiation.
b. Moderate change – for drug products change to equipment of the
same design and operating principle.
c. Minor change – in an existing code imprint for dosage form for
example changing from a numerical code to alphanumeric codes.
4. SPECIFICTION –
Conformance t o a specification means that the material when
tested according to the analytical procedures listed in the
specification will meet the list changed acceptance criteria.
5. PACKAGING CONTAINER-
MAJOR MODERATE MINOR
• For liquid and • A change in the • A change in the
semisolid dosage number of units size and shape of
forms a change in • e.g. ( tablet, a container for a
packaging capsule, or non sterile solid
materials (e.g. labeled amount(In dosage form.
plastic rubber) of gram or
primary milliliters.
packaging
components.
• Single unit dose
container to
multiple dose
container.
6. LABELLING –
MAJOR MODERATE MINOR
• based on post • Change in the • Change in the
marketing clinical study lay out of
study results, section packaging,
labeling reflecting new FDA
changes or modified regulation
associated data. editorial
with new changes, such
indication and as adding a
usage. distributors
name .
❑COMBINATION PRODUCT:-
Combination product is a product composed of a drug and a
device; a biological product and device; a drug and a biological
product.
➢ Examples:-
1. monoclonal antibody combined with a therapeutic drug.
2. Device coated or impregnated with a drug or biologic.
3. Catheter with antimicrobial coating, transdermal patch, pacing
lead with steroid coated tip.
4. Prefilled drug delivery system (syringes insulin injector pen,
metered dose inhaler).
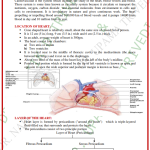
❑ MEDICAL DEVICES:-
• Medical devices are instrument apparatus, implement machine,
contrivance implant, in vitro reagent or other similar or related
article including any component, part or accessory.
• medical device doesn’t achieve its primary intended purposes
through chemical action within or on the body of man or other
animal and which is not dependent upon being metabolized for the
achievement of its primary intended purpose.
• In US FDA 3 assigned centers for regulation-
1. (CDER) (For combination product ) center for drug evaluation
and research.
1. Center for biologics evaluation and research.(CBER)
2. Center for devices and radiological health. (CDRH)
EXAMPLE
Wound dressing with antimicrobial- typically a device (CDRH).
Asthma inhaler or medicinal patch – typically a drug (CDER).
❑ DEVICE REGULATION
•FDA’s Center for Device and Radiological (CDRH) is main
regulatory body for manufacture, repack, relable or import of
medical device sold in the US.
• 1700 Different type of generic device into 16 medical specialties
referred as panel.
• Classification of medical device- on the basis of risk associated
with medical device it is classified as,
1. Class I device exempted from premarket notification (lowest
risk).
2. Class II devices require premarket notification. (Moderate risk).
3. Class III devices require premarket approval (high risk).
Class I
Class III
The basic regulatory requirements that manufacturers of medical
devices distributed in the US must comply
1. Establishment Registration
• Manufacturer/ importers must register their establishment with
FDA.
• Information verified annually between 1st oct -31st dec.
2. Medical Device listing
• Manufacturer must list their devices with FDA with
information about manufacturer, distributer, accessories,
remanufacturer, US manufacturer of ‘export only’ devices.
3. Premarket notification
• Letter of substantial equivalence from FDA requires before
commercial distribution.
4. Premarket approval (PMA)
• class III devices are high risk devices so they include the
submission of clinical data to support claims made for
the device.
• They are substantially not equal to predicate device.
5. Investigational device exception (IDE)
• Allows the investigational device to be used in a
clinical study in order to collect safety and effectiveness
data required to support a premarket.
• Clinical studies with devices of significant risk must be
approved by FDA and by an Institutional Review
Board (IRB) before the study can begin.
6. Quality system regulation (QC)/ Good Manufacturing
Practice(GMP)
• Includes methods, facilities and controls used for: designing,
purchasing, manufacturing , packaging, labeling, storing,
installing and servicing of medical devices to assure
compliance.
7. Labeling
• includes label on the device as well as descriptive
information literature that accompanies I the device.
8. Medical device reporting
• To identify and monitor significant adverse events involving
medical devices.
❖REGULATION OF COMBINATION PRODUCT
Combination products for human are regulated by 3
centers-
1. CBER(Center for biologics evaluation and research).
2. CDRH (Center for drug radiological health).
3. CDER (Center for drug evaluation research).
Center with primary regulatory (the lead) for a
combination product is determined based upon primary
mode of action of that compound.
PMOA:- it is defined as the mode of action, which
provides greatest contribution to the overall therapeutic
effect of the combination product.
CBER leads if the biologics has the PMOA.
CDRH leads if the device has PMOA.
CDER leads if the drug has the PMOA.
And these center review the products as IND and IDE if
it is class 1 device.
Premarket review.
Post market review.
▪ US FDA Office of Combination Products (OCP) is a
statutory mended office for regulatory affairs in combination
product.
▪The role of OCP:
1. Classifies and assigns therapeutic products.
2. coordinates and oversees regulation of combination products.
3. Facilitate meetings between sponsors and review staff.
4. Help resolve product class and product specific combination
product concerns.
5. Help resolves disputes between centers or with sponsors.
❑ The conformity assessment is done by the US FDA centers
1. Based on safety and effectiveness- constituents parts and
interaction of constituents parts.
2. Combined decision – making by centers, with OCP input as
needed.
3. Varying pathways to market depending on technology and
PMOA (primary modes of action, assigned lead center). The
conformity assessment is done by the US FDA centers.
4. Consistent procedure and standards to review process
❑ pre-market review process:
1. constituent part and interaction in between.
2. Combined analysis and decision by center.
3. consistent procedure and standards review process.
❑ marketing application:
1. application research required prior marketing.
2. Ongoing reliance on proprietary data.
3. Appropriate coordination of post marketing changes to
constituents parts
REFERENCES:
1. Shargel Leon , Generic Drug Product Development solid oral
dosage form, second Edition, volume 129, published by CRC
Press Taylor and Francis Group Boca Raton London, year
2014, page no.306-311
2. Berry Ira R. and Martin Robert P., The Pharmaceutical
Regulatory Process , second edition, volume 2 ,published by
Informa Healthcare USA, year 2008, page no 411-420.
3. http://www.fda.gov/medicaldevices/deviceregulation
guidance/overview/default.htm.
4. Mantus David S, Pisano Douglas J, FDA Regulatory Affairs,
second edition, year 2008 by Infprma Healthcare New York,
p.n. 187- 213.