1
ABSORPTION OF DRUGS
M.PHARM I YEAR,
DEPARTMENT OF PHARMACEUTICS,
COLLEGE OF PHARMACY,
2
CONTENTS
➢ DEFINITION
➢ INTRODUCTION
➢ STRUCTURE OF CELL MEMBRANE
➢ MECHANISM OF DRUG ABSORPTION
➢ FACTORS AFFECTING ABSORPTION
PHYSIO-CHEMICAL FACTORS
PHARMACEUTICAL FACTORS
➢ DOSAGE FORMS
➢ REFERENCES
INTRODUCTION OF ABSORPTION
3
Definition:
➢ Absorption can also be defined as the process of movement
of unchanged drug from the site of administration into the
systemic circulation.
➢ Concentration can be measured more accurately in plasma.
In drug absorption two parameters are frequently used.
➢ Magnitude of drug that reaches the systemic circulation
➢ Rate at which the drug is absorbed.
CELL MEMBRANE STRUCTURE
4
➢ Also called the plasma membrane, plasmalemma or
phospholipid bilayer.
➢ The plasma membrane is a flexible barrier that surrounds &
contains the cytoplasm of a cell.
➢ Cell membrane mainly consists of:
1.Lipid bilayer -phospholipid
-Cholesterol
-Glycolipids.
2. Proteins – Integral membrane proteins
-Lipid anchored proteins
-Peripheral Proteins
Hydrophobic core of the membrane is responsible for the
relative impermeability of polar molecules.
GI lining constituting the absorption barrier allows most nutrients
like glucose, amino acids ,fatty acids, vitamins, etc. 5
The basic structural framework of the plasma membrane is the
lipid bilayer.
This forms a continuous, spherical lipid bilayer app. 7nm thick.
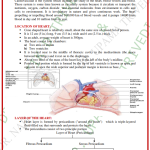
GASTRO INTESTINAL TRACT
6
STOMACH :
➢ The surface area for absorption of drugs is relatively small
in the stomach due to the absence of macrovilli &
microvilli.
➢ Stomach emptying applies more to the solid dosage forms
because the drug has to dissolve in the GI fluid before it is
available for absorption.
➢ Since solubility & dissolution rate of most drugs is a
function of pH.
SMALL INTESTINE :
7
❖ It is the major site for absorption of most drugs due to
large surface area.
❖ The blood flow to the small intestine is 6 to 10 times that
of stomach.
❖ Peristaltic movements of intestine is slow, transit time is
long, permeability is high.
➢ The transit time in small intestine for most healthy adults
is between 3 to 4 hours, a drug may take about 4 to 8
hours to pass through the stomach & small intestine
during fasting state.
➢ During the fed state, the small intestine transit time may
take about 8 to 12 hours.
LARGE INTESTINE :
8
❖ The length and mucosal surface area is very small
compared to small intestine so absorption of drug
from this region is insignificant.
❖ The main role is absorption of water and
electrolytes.
❖ Because of long residence time (6 to 12 hours)
colonic transit may be important in the absorption
of some poorly soluble drugs and sustained release
dosage forms.
MECHANISM OF DRUG ABSORPTION
9
There are three main mechanisms of drug transport across the
gastrointestinal epithelium.
➢ Trans cellular, i.e., Across the cells
Passive transport
Active transport
➢ Para cellular, i.e., Between the cells Pore transport
Permeation through tight junctions of epithelial cells
Persorption
➢ Vesicular i.e., Within the vesicles into cells.
Pinocytosis
Phagocytosis
TRANSCELULAR /INTRACELLULAR
The passage of the drugs across the GI epithelium is the 10
common pathway for the drug transport.
3 steps:
➢ Permeation of GI epithelial cell membrane, a lipoidal
barrier is the major obstacle to drug absorption.
➢ Movement across the intracellular space (cytosol).
➢ Permeation of the lateral or baso lateral membrane .
Passive transport process
➢ Passive diffusion
➢ Carrier mediated transport
➢ Facilitated diffusion
➢ Ionic electrochemical diffusion
➢ Ion pair transport
Passive Diffusion
11
It is defined as the
difference in the drug
concentration on either
side of the membrane.
Also called nonionic
diffusion
It is the major process for
absorption of more than
90% of the drugs.
The driving force for this
process is the
‘concentration or
electrochemical gradient’.
➢ Expressed by Fick’s first law of diffusion – 12
“The drug molecules diffuse from a region of
higher concentration to one of lower
concentration until equilibrium is attained & the
rate of diffusion is directly proportional to the
concentration gradient across the membrane”.
dQ = D A Km/v (CGIT – C)
dt h
Cntd…
Where, 13
dQ/dt = Rate of diffusion (Amount/time)
D = Diffusion co efficient of the drug
through the membrane( Area/time)
A = Surface area of the absorbing membrane
for drug diffusion(Area)
Km/w = Partition co efficient
Cgit – C = Concentration gradient
h = Thickness of the membrane
Pore Transport
It is also called as Convective transport, Bulk flow1 4
or filtration.
Mechanism – Protein channels present in the cell
membrane.
The driving force for this process is the ‘hydrostatic
pressure or the osmotic differences across the
membrane’.
The process is important in the absorption of low
molecular weight (less than 100), low molecular
size drugs.
Example: Urea, Water, Sugar
15
➢ The rate of absorption via pore transport depends on the
number & size of the pores, & given as follows:
dc = N R 2 A ∆C
dt (η) (h)
where,
dc /dt = rate of the absorption.
N = number of pores
R = radius of pores
∆C = concentration gradient
η = viscosity of fluid in the pores
Two types
16
Facilitated diffusion
Active transport
Facilitated diffusion
➢ This mechanism involves the driving force is
concentration gradient.
➢ In this system, no expenditure of energy is involved
(down-hill transport), therefore the process is not
inhibited by metabolic poisons that interfere with
energy production.
➢ Eg. Vitamin B12.
Active transport
17
➢ Transport process
require energy from
ATP to move drug
molecules from
extracellular to
intracellular fluid.
➢ It is process where the
materials are transported
across membranes
against a concentration
gradient.
➢ The drug is transported from a region of lower to
one of higher concentration i.e.. against the 18
concentration gradient or ‘uphill transport’.
➢ Examples : Sodium, potassium, iron, glucose and
vitamins like niacin, pyridoxine and ascorbic acid.
Types
➢ Primary active transport –Uniport
❖ Ion transporters
❖ ABC (ATP – binding cassette ) transporters –
Eg: p Glycoprotein. MDR.( Multi drug resistance)
➢ Secondary active transport
❖ Symport (co -transport)
❖ Antiport (counter -transport)
Paracellular/IntercellularTransport 19
➢ It is defined as the transport of drugs through the junctions
between the GI epithelial cells. This pathway is of minor
importance in drug absorption. The two paracellular
transport mechanisms involved in drug absorption are –
➢ Permeation through tight junctions of epithelial cells –
this process basically occurs through openings which are
little bigger than the aqueous pores. Compounds such as
insulin and cardiac glycosides are taken up this
mechanism.
➢ Persorption – is permeation of drug through temporary
openings formed by shedding of two neighbouring
epithelial cells into the lumen.
Endocytosis
20
➢ Also called Corpuscular or Vesicular transport
➢ It involves engulfing extracellular materials within a
segment of the cell membrane to form a saccule or a
vesicle which is then pinched-off intra cellularly.
➢ Includes two type of process:
Phagocytosis (cell eating): adsorptive uptake of solid
particulates, and
Pinocytosis (cell drinking): uptake of fluid solute.
➢Fats, starch, vitamins like A, D, E, K
FACTORS AFFECTING DRUG
21
ABSORPTION
(a)PHARMACEUTICAL FACTORS
Physicochemical Factors
Dosage form characteristics
(b)PATIENT RELATED FACTORS
Physicochemical factors 22
➢ Lipid solubility ,dissociation constant and pH
➢ Dissolution
➢ Salt form
➢ Particle size and Effective surface area
➢ Polymorphism and Amorphism
➢ Solvates and hydrates(Pseudopolymorphism)
➢ Salt form
➢ Drug permeability and absorption
➢ Viscosity
Lipid solubility and dissociation constant and 23
pH
More the drug in non ionized form , more is it lipid
soluble and better is the absorption.
pH partition hypothesis
The interrelationship of dissociation
constant, lipid solubility,pH at the absorption site
and absorption characteristics of various drugs
throughout the GIT.
The pH partition theory is the process of drug 24
absorption from the GIT and its distribution across
all biological membrane.
The theory states “ That for the drug compound of
molecular weight greater than 100 , which are
primarily transported across the bio membrane by
passive diffusion , the process of absorption is
governed by
➢ Dissociation constant
➢ Lipid solubility
➢ pH at the absorption site
25
The rate of loss of drug in solution form from the
absorption site is given by:
-DCt/dt = KaCu
Ct
Where,
Dct/dt= rate of drug loss from absorption site
Ka = absorption rate constant
Ct =Total drug concentration
Cu = concentration of unionized drug.
The dissociation constant is expressed for both acids
and bases as a pKa value: 26
➢ FOR ACID
pH= pKa +log conc.(ionized)/conc.(unionized)
➢ FOR BASE
pH= pKa +log conc.(unionized)/conc.(ionized)
Weakly acidic drugs (Eg :Aspirin) dissolve faster in
gastric fluids.
Weakly basic drugs (Eg :Quinine) dissolve faster in
intestinal fluids.
Acidification or basification of both stomach and
intestine will produce converse effects.
Dissolution
27
Drug gets absorbed in the biological system, when it gets
dissolved in the physiological fluid at the absorption site.
Solid dosage form(tablet or capsule)
Disintegration(coarse particles of drug)
Dissolution
Drug in solution(very fine particles)
Drug in systemic circulation
Dissolution
28
Theories of drug dissolution
29
➢ Diffusion layer model/film theory
➢ Danckwert’s model/surface renewal theory
➢ Interfacial model/double barrier model theory
Salt form
30
➢ Conversion of a weakly acidic or basic drug in its salt
form enhances the solubility and dissolution rate of the
drug.
➢ Weakly acidic drug- strong base salt
Eg. Na, K salts of barbiturates, sulphonamides
➢ Weakly basic drug- strong acid salt
Eg. Hcl,SO4 salts of alkaloidal drugs.
Particle size and surface area
➢ Particle size and surface area share an inverse
relationship.
➢ Surface area can be classified as
(1)Absolute surface area
(2)Effective surface area
➢ Greater the effective surface area, better the disso3lu1tion
and so the absorption.
➢ Absolute surface area can be converted to effective
surface area by :
(1)Use of surfactants like Polysorbate 80.
(2)Adding hydrophillic diluents like PEG,PVP etc.
Polymorphism and amorphism
POLYMORPHISM
-Substances exist in more than one crystalline form
-Definite structural arrangements
-Different physical properties :
Density, Melting point, Boiling point, solubility.
Two types
Enantiotropic – reversible-altering temp & pressure. 32
Eg. Sulphur
Monotropic – unstable at all temp & pressure.
Eg. Glyceryl stearates
STABLE – ↑Melting point ↓energy ↓solubility
METASTABLE – ↓Melting point ↑energy ↑ solubility
↑ bioavailability
AMORPHISM
No internal crystal structure ↑ aqueous solubility
Eg. Novobiocin- amorphous form 10 times more soluble
than crystalline form.
Dissolution: Amorphous>meta stable >Stable
33
INTERNAL STRUCTURE OF A
COMPOUND
CRYSTALLINE
AMORPHOUS
NON STOICHOMETRIC
MOLECULAR
POLYMORPHS
ADDUCTS
STOICHOMETRIC(PSEUDOPOLYMORPHS)
ENANTIOTROPIC MONOTROPS
ORGANIC
HYDRATES
SOLVATES
Hydrates and solvates 34
SOLVATES
➢ Adducts where solvent molecule incorporated in
crystal lattice of solid
➢ High solubility
➢ Eg. Solvates of Cortisone , Griseofulvin
HYDRATES
➢ If solvent is water – called as hydrate
➢ Anhydrous forms more soluble than hydrates
➢ Eg. Anhydrous ampicillin , Theophylline
Drug permeability and absorption 35
➢ Most orally administered drugs enter the systemic
circulation by passive diffusion
➢ Three major characters that determine the
permeability of the drug across the intestinal
epithelium are:
(A) Lipophilicity of the drug
(b) Polarity
(c) Molecular size
➢ The net effect of above three properties is given as
36
RULE OF FIVE by Lipinski which is written as:
Molecular weight of drug <=500
Lipophilicity of drug <=5
Number of H-bond receptors <=10
Number of H-bond donors <=5
❑ If any two of these values are greater than
specified limits, the oral absorption of a drug may
be a significant problem.
Drug stability
37
A drug for oral use may destabilized either during
its shelf life or in the GIT.
Two major stability problems resulting in poor
bioavailability of an orally administered drug are –
degradation of the drug into inactive form, and
interaction with one or more different component(s)
either of the dosage form or those present in the
GIT to form a complex that is poorly soluble or is
unabsorbable.
Pharmaceutical factors 38
➢ Disintegration time
➢ Dissolution time
➢ Manufacturing and processing variables
Method of granulation
Compression force
➢ Pharmaceutical ingredient/excipients
Disintegration time
➢ Rapid disintegration is important to have a rapid 39
absorption so lower disintegration time is required.
➢ Disintegration time of tablet is directly proportional to
amount of binder and compression force.
Dissolution time:
➢ Dissolution is a process in which a solid substance
solubilises in a given solvent i.e, mass transfer from
the solid surface to the liquid phase.
➢ Dissolution time is also an important factor which
affect the drug absorption .
Manufacturing variables:
40
➢ Several manufacturing processes influence drug
dissolution from solid dosage forms.
For example: For tablet it is
➢Method of granulation
➢Compression force
Method of granulation:
➢ Different methods like wet granulation , dry
granulation and direct compression etc. yields
product with different dissolution.
Compression force
The compression force employed in tableting4 1
process influence density, porosity, hardness,
disintegration time and dissolution rate of tablets.
Pharmaceutical ingredients/excipients:
More the number of Excipients in the dosage form,
more complex it is & greater the potential for
absorption and Bioavailability problems.
A) Vehicle
Rate of absorption – depends on its miscibility with
biological fluid.
Miscible vehicles (aqueous or water miscible
vehicle) causes rapid absorption e.g. propylene
glycol.
Immiscible vehicles – Absorption depends on its
partitioning from oil phase to aqueous body fluid. 42
B) Diluents
Hydrophilic diluents – Imparts Absorption
Hydrophobic diluents – Retards Absorption
Also, there is a drug-diluent interaction, forming
insoluble complex and retards the absorption. E.g.
Tetracycline-di calcium phosphate
C) Disintegrants
Mostly hydrophilic in nature.
Decrease in amount of disintegrants – significantly
lowers B.A.
D) Binders & granulating agent –
Hydrophilic binders – Imparts hydrophilic 43
properties to the granule surface – gives better
dissolution properties of the poorly wettable drugs.
E.g. Starch, Gelatin,PVP.
But more amount of binder increases the hardness
of the tablet and retards the absorption rate.
E) Suspending agents/viscosity agent
Stabilized the solid drug particles and thus affect
drug absorption.
Macromolecular gum forms un-absorbable complex
with drug eg. Na CMC.
Viscosity imparters – act as a mechanical barrier to
diffusion of drug from its dosage form and retard GI
transit of drug.
F) Surfactants
May enhance or retards drug absorption by interacting 4w4ith
drug or membrane or both.
Physiologic surfactants – bile salts – promotes absorption –
e.g. Griseofulvin, steroids
It may decrease absorption when it forms the un-absorbable
complex with drug above CMC.
G) Coating
In general, deleterious effects of various coatings on the drug
dissolution from a tablet dosage form are in the following
order.
Enteric coat > sugar coat > non-enteric coat.
The dissolution profile of certain coating materials change on
aging; e.g. shellac coated tablets, on prolonged storage,
dissolve more slowly in the intestine. This can be however,
be prevented by incorporating little PVP in the coating
formulation.
H) Lubricants 45
Commonly hydrophobic in nature – therefore
inhibits penetration of water into tablet and their
dissolution and disintegration.
I) Colourants
Even a low concentration of water soluble dye can
have an inhibitory effect on dissolution rate of
several crystalline drugs.
The dye molecules get absorbed onto the crystal
faces and inhibit the drug dissolution. Eg:Brilliant
blue retards dissolution of sulfathiazole.
Nature and type of dosage form
46
Apart from the proper selection of the drug, clinical
success often depends to a great extent on the proper
selection of the dosage form of that drug.
As a general rule, the bio-availability of a drug form
various dosage forms decrease in the following order:
Solutions > Emulsions > Suspensions > Capsules >
Tablets > Coated Tablets > Enteric Coated Tablets >
Sustained Release Products.
Product age and storage conditions:47
Product aging and storage conditions can adversely
affect the bio-availability by change in especially
the physico-chemical properties of the dosage
forms.
For example:
Precipitation of the drug in solution
Hardening of tablet
Change in particle size of suspension.
Dosage forms
➢ Order of bioavailability of drugs. 48
➢ Solutions>suspensions>capsules>tablets>coated
tablets
SOLUTIONS
➢ Drugs absorbed more rapidly in this form.
➢ When this formulation is taken after meal gastric
emptying is the rate limiting step.
Factors influencing are
➢ Nature of the solvent(aqueous, water miscible)
viscosity, surfactant, solubilisers, stabilizers.
➢ Drugs which are poorly soluble can be converted
to water soluble by the addition of co solvents
such as alcohol, propylene glycol, polyethylene
glycol 400 etc…
ELIXIRS SYRUPS 49
1. Elixirs are sweetened 1. Syrups are concentrated
aromatic hydro-alcoholic aqueous preparation of
preparations. sugar.
2. Less effective and less 2. More effective and more
sweeter than syrup sweeter than elixir.
3. Less viscous due to 3. More viscous than
containing low elixirs.
proportion of sugar.
E.g:Chlorpheniramine E.g Paediatric Paracetamol
elixir syrup
Suspensions
50
➢ Dissolution is the rate limiting step for the
absorption the drug from suspension.
Factors to considered are
➢ Particle size ,
➢ Wetting agents,
➢ Viscosity of the medium,
➢ Suspending agent
➢ E.g: Chloramphenicol suspension
Capsules
51
For hard gelatin capsules the shell should disrupt
quickly and expose the contents to the GI fluids.
Factors influencing are particle size, density, crystal
form of the drug, selection of diluents.
soft elastic capsule dissolve faster than hard gelatin
capsule & tablets. Which shows better bioavailability
from oily solutions, emulsions, or suspensions.
Tablets
52
This is the most widely used dosage form.
Problem with this arises from reduction in the effective
surface area due to granulation& subsequent
compression in to dosage form.
Tablet disintegration and granule disintegration are the
important steps in absorption process.
Compression force also may be an important factor.
Disintegration is the rate limiting step for this.
E.g: Riboflavin tablet.
Coated tablets
➢ Coat is generally used to mask unpleasant taste & 53
odor & to protect the ingredients from decomposition
during storage.
➢ This adds an additional barrier between GIT & drug.
It should get dissolve before tablet disintegration &
dissolution.
Sugar & film coatings
➢ Sugar coating will take more time than film coating.
➢ Ex: methyl cellulose which retards the dissolution
➢ Now a days film and press coated are mostly used.
Enteric coated tablets
54
➢ It is a special film coated design to restricts the
gastric fluids & to dissolve in small intestine.
➢ Protect the drug from the degradation in the stomach
Ex: erythromycin.
➢ Minimize the gastric distress caused by some drugs.
Ex: aspirin.
➢ These tablets must empty the stomach before the drug
absorption can begin.
➢ The polymers with pka values ranging from 4-7 have
been found to use.
➢ E.g: Diclofenac enteric coated tablet.
REFERENCES:
55
➢ D.M. Brahmankar, S.B. Jaiswal; “Bio pharmaceutics
& Pharmacokinetics”; first edition, 12th reprint;
VallabhPrakashan;
➢ MiloGibaldi ; “Bio pharmaceutics and clinical
pharmacokinetics “ fourth edition , Pharma Med
Press.
➢ “Clinical pharmacokinetics ,concepts and
applications “ 3rd edition by Malcom Rowland and
Thom N .Tozer, Lea febiger.
➢ “Applied Bio pharmaceutics & Pharmacokinetics”
by Shargel ,Land Yu ABC, 2nd edition.
56
THANK
YOU