Pharmacology Team
Anti-Coagulants
Done by:
*Jumana AlShammari.
* Ibrahim Al-Gamdi.
Introduction: The introduction is just for
your information. Thanks to
Hemostasis refers to the finely regulated dynamic process of maintaining fluidity of Pharmacology Team 430
blood, repairing vascular injury, and limiting blood loss while avoiding vessel occlusion
(thrombosis) and inadequate perfusion of vital organs. Either extreme—excessive bleeding or thrombosis—represents a
breakdown of the hemostatic mechanism.
Blood vessel injury triggers the following sequence:
• The vessel constricts to reduce blood flow
• Circulating platelets adhere to the vessel wall at the site of trauma
• Platelet activation and aggregation, coupled with an intricate series of enzymatic reactions involving
coagulation proteins, produces fibrin to form a stable haemostatic plug.
Antithrombotic drugs are used for prevention and treatment of thrombosis. Targeting the components of thrombi, these
agents include (1) antiplatelet drugs, (2) anticoagulants, and (3) fibrinolytic agents. With the predominance of platelets
in arterial thrombi, strategies to inhibit or treat arterial thrombosis focus mainly on antiplatelet agents, although, in
the acute setting, they often include anticoagulants and fibrinolytic agents.
Anticoagulants are the mainstay of prevention and treatment of venous thromboembolism because fibrin is the
predominant component of venous thrombi. Antiplatelet drugs are less effective than anticoagulants in this setting
because of the limited platelet content of venous thrombi.
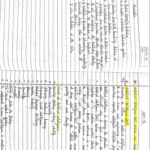
The factor needs calcium
Anticoagulants: Collagen Activated Platelets
The factor depends on vit K
Coagulation cascade:
http://www.youtube.com/watch?v=MPGe-‐guZMqM Intrinsic Path
essel Injury way
12 a Blood v
Clotting: slower / accessed
http://www.youtube.com/watch?v=iU-‐ by aPTT
P5nyD8AQ&feature=related 11 a
APPT
Extrinsic pathway
Clotting: is rapid in Heparin
sec. / accessed by PT 9 a LMWH
8 a
PT
Warfarin
Tissue injury
Activates the tissue 7 a 10a
5 a Direct factor 10a inhibitor
Factor which then
activates
Thrombin (2a) Direct thrombin inhibitor
Fibrin 13 a
Stabilized fibrin
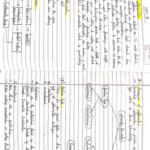
Anticoagulant
Works best on venous thrombosis than arterial thrombosis (can be used as 2nd line after anti-platelet)
Parenteral Anticoagulant Oral Anticoagulant
(Used in acute ‘emergency’ Cases)
Unfractiona LMW Direct Thrombin Factor Xa Vitamin K
ted heparin Heparin inhibitors Inhibitor antagonist
Molecule 3000-30000 < 8000 Pentasaccharide
weight
XIIa, XIa, IXa, Xa, IIa Thrombin 2a Factor Xa Factors II, VII, IX
And thrombin & X
(1000 more potent than Anti
Acts on thrombin3)
Works
more on
Xa
Heparin Enoxaparin Reversible: Indirect: Coumarins:
Lovenox • Bivaluridin Fondaparinux
Dalteparin • Argatroban Ø Warfarin
• Dabigatran Direct: > 40 times
Rivaroxaban potency than
Irreversible: Which is taken Ø Dicumarol
• Lepirudin Orally
Drugs
Ø Irreversible is more
dangerous
It’s not
It’s not important to important to
know which is know which is
reversible/irreversible Direct/Indirect
Inactivation of Coagulation Factors by Anti-thrombin III Decrease
MOA Synthesis
Pharmacokineti • Rapid • Slow
cs • Variable (unpredictable) • Latency
• Variable
• aPTT (1.5 – 2.5 times normal [30sec]) • PT (2 times)
Monitor • CT (2-3 times normal [5-7 min]) • INR (2.5)
• Protamine Sulphate IV 1mg for each 100 units UFH • Vitamin K1
• Fresh blood infusion
Antidote • Fresh blood
• Needs de novo
synthesis
APTT: Activated partial thromboplastin time test is a laboratory test used to monitor the anticoagulant effect of unfractionated
heparin and direct thrombin inhibitors; prolonged when drug effect is adequate.
Prothrombin time (PT) test: Laboratory test used to monitor the anticoagulant effect of warfarin; prolonged when drug effect
is adequate
INR: It is a laboratory test that measure the time it takes for blood to clot and compares it to an average.
Notes:
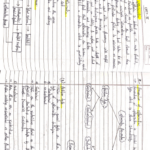
• Unfractionated heparin inhibits both antithrombin 2a and Factor Xa equally.
• Low Molecular Weight heparin inhibits Factor Xa more (double) than Antithrombin 2a
v Both can cause recurrence of thrombosis (does not inhibit the fibrin bound thrombin)
• Direct thrombin inhibitors works only on the fibrin bound thrombin (no re-thrombosis)
Unfractionated Heparin Limitations:
• No predictable anticoagulant effects: inter-patient & intra-patient variability in response to a given
dosage in hospital setting, repeated monitoring
• Low bioavailability binds to plasma proteins, endothelium & macrophages
• Re-thrombosis activates platelets & it does not neutralize fibrin-bound II a (usually occurs
after 1 day or less)
• Heparin Induced Thrombocytopenia (HIT): In 4% pts. On heparin Venous > Arterial thrombosis
• Latency:
• 5-10 days after 1st exposure
• Or 2-3 days after re-exposures
• Signs:
• Thrombocytopenia AND Thrombosis
• Treatment
• Heparin Disconnection
• No Packed Platelets à will cause more
thrombosis
• No Warfarin à will cause venous
gangrene
• GIVE Direct Thrombin Inhibitors
Comparison between Unfractionated Heparin and Low Molecular Weight Heparin
Low Molecular Weight Heparin Benefits:
• Predictability of anticoagulant response i.e. little inter-patient and intra-patient variability in
response to a given dosage. So effective anticoagulant activity can be achieved by calculating
dosages based on body weight without the need for laboratory monitoring
• Bioavailability: as it hardly binds to plasma proteins, endothelium &
macrophages
• ¤Incidence of thrombocytopenia: as it seldom sensitive to PF4
• ¤Incidence of bleeding tendency: ¤ effect AT III & ¤ platelet interactions
• Much better tolerability:
§ Given subcutaneous
§ ¤ Frequency of administration due to longer duration of action
§ ¤ Need for regular monitoring
§ Outside hospital settings
Vitamin K Antagonists:
Precursors of factors II, VII, IX & X require carboxylation of their glutamic a. residues to allow them to
bind to phospholipid surfaces. Vitamin provides this. K as it changes from its oxidized to its reduced form.
Instantaneously, the reduced Vitamin K has to recycle back to oxidized form by Vitamin K epoxide
reductase. This enzyme is blocked by VKAs losing the coagulation factors the ability to function.
Vitamin K Antagonists Limitations:
• Wide variation in drug response a necessity for continuous monitoring (PT) and INR & dose
adjustment
• Has narrow therapeutic window; high Plasma Protein Bound & action depends on very small
fraction of free drug. So any change in that level can be hazardous.
• Slow onset of action, so NOT in given in emergency conditions
• Has latency in its action presents the time needed to launch new biologically inactive
coagulation factors
• Common genetic polymorphism in CYT P450 isoforms that metabolizes warfarin adds to its
non-predictable response liability to toxicities or under use.
• Numerous food- & drug-drug interactions liability to toxicities or under use.
• Contraindicated in some conditions liable to develop thrombosis i.e. as in PREGNANCY give
heparin or LMWH instead
Factors Altering Response To VKAs: Not Important
Increasing Factors:
1. Vitamin K deficiency;
a- Inadequate diet: malnutrition, dieting,….
b- Inadequate absorption: diseases of small intestine, diseases ¤ biliary secretion
2. Impaired synthesis of clotting factors;
a. In hepatocellular disorders: (hepatitis; viral, autoimmune, drug-induced, chronic
alcoholism … etc.)
b. In hepatic congestion: in congestive HF…etc)
3. Increased catabolism of clotting factors;
In hypermetabolic states: as in fever, thyrotoxicosis
Decreasing Factors:
1. Decreased plasma protein binding;
£ elimination of free drug & shortening of its t1/2. as pts with nephrotic syndrome (proteinuria)
2. Decreased catabolism of clotting factors; Hypothyroidism
3. Hereditary resistance to oral anticoagulants
VERY IMPORTANT You should know the
Drugs Modulating Response To VKAs: drugs and how they modulate VKAs
Drugs that increase INR:
1. Inhibition of Vitamin K synthesis by intestinal flora: oral antibiotics
2. Inhibition of Vitamin K absorption: liquid paraffin
3. Decrease in drug metabolism by microsomal enzyme inhibitors: chloramphenicol, &
cimetidine
4. Displacement of the drug from protein binding sites: phenylbutazone & salicylates
5. Co-administration of drugs that increase bleeding tendency by:
§ Inhibiting platelet function: NSAIDs
§ Inhibiting coagulation factors: heparin
Drugs that decrease INR:
1. Inhibition of drug absorption from GIT: cholystyramine, colestipol
2. Increase in synthesis of clotting factors: Vitamin K, oral contraceptives
3. Increase in drug metabolism by microsomal enzyme inducers: carbamazepine,
rifampicin
Cases:
Case 1: An old, peptic ulcer patient, sustained on cimetidine, has been bed ridden since a month following a
major orthopedic surgery for pelvic fracture. The last week he began to complain of pain, tenderness,
warmth & swelling of his left leg. He was diagnosed as deep vein thrombosis. His treating physician
put him first on heparin that was replaced after three days by VKAs. Today he began to show
bleeding of gums.
What is the expected explanation of his finding?
VKAs toxicity due to interaction with cimetidine which is an enzyme inhibitor
Will the treating physician 1st of all, consider giving an antidote to stop bleeding (if so then state) or
will he probably ask for lab investigation (if so then state)?
No need for an antidote or blood transfusion because it is minor bleeding
Once lab findings are there, is the physician expected first to withdraw or to adjust the existing
therapy?
Gum bleeding is considered as a mild bleeding, so Dose adjustment is enough.
Case 2: A young rheumatic artheritic patient has undergone valve replacement and is sustained on warfarin
therapy for the last three years. When she married, last summer, she did not want to get pregnant, so
she has taken since then, oral contraceptive pills. Her regular lab monitoring today showed a
decrease in INR this time.
What is the expected explanation of her lab result?
Since the patient is taking oral contraceptive there will be an increase in synthesis of clotting factors
reducing the efficacy of the warfarin
What will the treating physician consider doing?
a) Giving heparin on top
b) Adjusting warfarin dose
c) Stopping the OC
d) Stopping warfarin
Answer is b
Case 3: A 53 years old patient had an aortic valve replacement since 5 years and he is sustained on
warfarin. A week ago, he developed low grade fever, diarrhea and was diagnosed as having
typhoid. He was given rehydration fluid and a course of chloramphenicol. Today he is complaining
from haematuria.
Which one of the following best explains the haematuria?
a) Inhibition of Vitamin K synthesis by chloramphenicol
b) Displacement of warfarin from protein binding site by rehydration
c) Decrease in warfarin metabolism induced by chloramphenicol
d) Inhibition of Vitamin K absorption caused by the diarrhea
Answer is c
Which is the right decision to do in such a case?
a) Give a urinary antiseptic for fear of infection
b) Stop administering the regular intake of warfarin
c) Adjust the dose of warfarin after monitoring the situation.
d) Stop the course of chloramphenicol intended for typhoid therapy
Answer is c
Summary
Anticoagulants are mainly used in treatment of venous thromboembolism while antiplatelets used mainly
in treatment of arterial thrombosis.
• Heparin : inactivate factors 12a ,11a ,9a, 10a , thrombin, and has a variable response monitored by PTT or
A PPT.
• – If there is toxicity à Antidote; Protamine Sulphate IV 1mg / 100 units UFH + Fresh blood
• – It does not inhibit the fibrin bound thrombin that’s why it has an incidence of causing re thrombosis.
st
– It also causes Heparin Induced Thrombocytopenia (HIT); latency 5-‐10 dys. after 1 exposure or 2-‐
3 dys After re-‐exposures if this occurs: Heparin withdrawn and give DTIs .No packed
platelets or
warfarin.
• Lower molecular weight heparin works more on inhibiting activated factor 10.It has Predictability of
anticoagulant response , Bioavailability , ¤Incidence of thrombocytopenia ,¤Incidence of bleeding
tendency and better tolerability than UFH
• Direct factor 10a inhibitors affects factor10a , monitored by APTT or PPT (they are the same)
• ·Direct thrombin inhibitors affect fibrin bound thrombin , monitored by PTT. It is the only drug that doesn’t
cause re thrombosis.
• Vitamin K Antagonists (warfarin) affects on the factors that depend on vit k which are 7a , 9 a , 10 a ,
t hrombin by inhibiting Vit K epoxide reductase. Monitored by PT due to its variable response.
• Contraindicated in pregnancy give heparin or LMWH instead
• Slow onset of action, so not in given in emergency conditions
– Metabolize in the liver by CYT P450 à Numerous food-‐ & drug-‐drug interactions.
Thanks to Pharmacology Team 430 For the introduction & summar
Question:
1- which one of the following is considered an advantage of low molecular weight heparin (LMWH)over unfractionated heparin?
a) has no sepecific antidote if bleeding occurs
b) is only given in a hospital setting.
c) has a predictable anticoagulant.
d) increase similar activation to antithrombine-‐111and Xa.
Answer : C
2- five years ago, a 53 year old patient had an aortic valve replacement and was sustained on warfarin. Two weeks ago, his lipid
profile showed hypertriglyceridemia for which he received clofibrate. Today he began to develop bleeding from the gums. Which
one of the following decisions should his treating physician consider?
a) stop the regular warfarin intake that he has been receiving for years.
b) Administer protamine sulphate intravenously as antidote.
c) stopthelipidloweringagentthatwasgivenrecently.
d) Ask for an INR and adjust the dose of warfarin accordingly.
Answer : D
3- A patient on oral anticoagulant therapy for treatment of deep vein thrombosis, developed severe gastroenteritis and was put on
rehydration therapy and a course of oral cephalosporin. Today, on lab checkup, the INR is high. Which one of the following
reasons is the likely cause of this lab finding?
a) inhibition of vitamin K synthesis by the suppressed intestinal flora.
b) displacemint of the anticoagulant from its protein binding site by the current treatment.
c) inhibition of absorption of vitamin K by cephalosporin.
d) increased bleeding tendency by activating the platelets by cephalosporin.
Answer : A
4- A patient previously on heparin developed thrombocytopenia and thrombosis on second exposure to the drug. He was
diagnosed as heparin induced thrombocytopenia. Which one of the following drugs can best treat such condition?
a) vitamin K antagonists.
b) directthrombininhibitors.
c) low molecular weight heparin.
d) anti-‐factor X inhibitors.
Answer : B